A 49 year old male with headache on the right hand side and severe giddiness since 2 months - GM CASE 20
30th June 2023
CASE STUDY 20
Hello, I am Saloni .S. Gangotri , a 5th semester medical student. This is an online elog book to discuss our patients health data after taking his/her consent. This also reflects my patient centered online learning portfolio.
CASE SHEET:
CHIEF COMPLAINTS:
c/o
- headache on the right hand side radiating to the face on the same side.
- severe giddiness in all positions.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 8 years back until he started developing headache on the right hand side of the skull which radiated to the face below on the same side accompanied by blurring of vision. He was brought to our hospital with the same complaints and was appropriately treated. 2 months back he developed same symptoms but this time along with on and off giddiness which makes him feel like he is falling down in almost all positions specially when he gets up from the lying down position.
He was taken to the nearby Bhuvanagari hospital where they changed his medication for diabetes mellitus to
a) Voglow GM2 forte - SR
b) Zoryl M3 forte and was sent back.
His symptoms continued which he somehow managed symptomatically. Until 10 days back while he was driving his autorickshaw he suddenly felt tired and dehydrated which he thought was because of the hot weather. He returned home, had his usual lunch and went off to sleep for around 2 -4 hours. After waking up he wasn't able to move any of his limbs and did not even recognise any sensation in them. He was taken to the Choutuppal hospital from where he was transferred to Bhuvanagiri hospital. Since the past 3 days he has a feeling of lacrimation in his right eye. He has had 3 episodes of self induced vomiting as a coping mechanism to giddiness. The vomitus was bilious and contained no food contents. He also had 3 episodes of loose motions which were watery and contained no blood. Since yesterday he has been complaining of facial puffiness. He has been having a stressful attitude since the past 2 months due to his daughter's marriage.
-h/o occasional burning micturition
-no h/o reduced urine output
-no h/o itching or rash.
-no h/o fever.
-no h/o cough with sputum.
-no h/o constipation.
-h/o 3 episodes of watery diarrhea.
-h/o headache and blurring of vision since the past 2 months.
-no loss of consciousness.
Earlier daily routine —
Earlier when the patient was asymptomatic he used to begin the day at 5am and used to start working.
At 9am he used to bathe and eat breakfast which consisted of rice and tea
Around lunch time if he was hungry, he consumed rice or coffee/tea whatever available as his lunch.
Around 8pm he used to have dinner containing rice and goes off to sleep. He consumed a bottle of thumbs-up soft drink everyday with dinner.
ASSOCIATED DISEASES:
———
PAST HISTORY:
h/o HTN which was diagnosed 10 days back in Choutuppal hospital. Is on irregular medication of Metaprolol + Chlorthalidone.
h/o Diabetes Mellitus since 13 years for which he used to regularly consume
a) Geminor M3 forte - PR twice daily
until 1 months back it was changed t
a) Voglow GM2 forte - SR and
b) Zoryl M3 forte.
No K/C/O TB, Epilepsy, CAD, CKD.
no h/o blood transfusions.
-h/o hemorrhoids surgery 20 years back.
PERSONAL HISTORY:
Married.
Resides in Choutuppal
Autodriver and farmer by occupation. He stopped farming 1 year ago.
On a mixed diet. Eats egg and consumed non-veg food only when wishes to.
Adequate sleep. but had a disturbed sleep yesterday night due to unknown reasons.
Has a normal appetite.
Normal Bowel movements.
Has no known allergies.
Used to smoke cigarretes in teenage but now stopped.
He was a chronic alcoholic and used to drink 1 bottle/ day but stopped 8 years back.
FAMILY HISTORY:
- h/o father having HTN and left hemiplegia.
Has N/K/C/O No Strokes. No CAD, TB, Asthma or Epilepsy.
DRUG HISTORY:
GENERAL EXAMINATION:
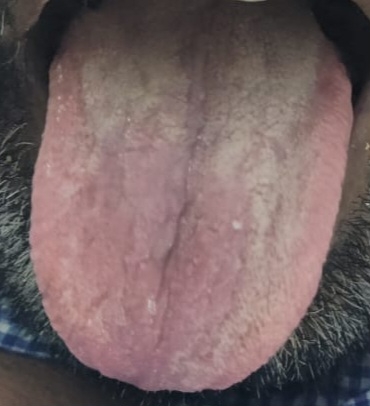
-No palor
-No icterus
-No cyanosis
-No lymphadenopathy
-No pedal edema
-No clubbing of fingers
VITALS:
Temperature: Afebrile - 98.9°F
Pulse: 60 beats per minute
Respiratory rate: —14 cycles per minute
Blood pressure: 170/100 mm of Hg
SPO²: 98%
GRBS: 428mg%
SYSTEMIC EXAMINATION:
Cardiovascular system:
No thrills
No murumurs
Cardiac sounds: S1, S2 present
Respiratory system:
Tracheal position: Central
No dyspnea
No wheezing
Breath sounds heard: vesicular? yes
Abdomen:
-Shape : Scaphoid
-No Tenderness present
-No palpable mass
-Non palpable spleen
-Non palpable liver
-No free fluid (ascites) present
-No bruits
-Bowel sounds: heard
Central Nervous System:
Conscious and Alert
Speech: Normal
INVESTIGATIONS:
Biochemical investigations:
ECG:
2D-ECHO REPORT:
ULTRASOUND REPORT:
GRAPHIC SHEET :
PROVISIONAL DIAGNOSIS:
———