A 74 year old male with grade IV SOB, recurrent high grade fever with chills and epigastric pain radiating to chest - GM CASE 19
29th June 2023
CASE STUDY 19
Hello, I am Saloni .S. Gangotri , a 5th semester medical student. This is an online elog book to discuss our patients health data after taking his/her consent. This also reflects my patient centered online learning portfolio.
CASE SHEET:
CHIEF COMPLAINTS:
c/o
- epigastric pain radiating to chest associated with belching.
- recurrent high grade fever for 4 days 6 days back associated with chills which was not relieved on medication.
- pedal edema since 8 days which is gradually reducing.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 15 years back when he developed fever with chills and grade IV SOB. He was hypotensive and had 1 episode of emesis which was bilious, non projectile and contained no food contents. He also said there was presence of black coloured blood clots in his stool. At the same time he also developed jaundice for which he consumed ayurvedic medicine and was relieved of symptoms. He visited a local practitioner for the above complaints and was diagnosed with Chronic Renal Failure. He was prescribed medicines for 6 months and regular dialysis which he escaped and consumed the medications for 3 years. Since then he has been doing okay and was on conservative management.
10 days back he developed a high grade fever associated with chills which was recurrent and not relieved on medication. He also developed severe epigastric pain which was radiating on the upper side towards the right side of the chest. This was accompanied by bloating, belching and was not relieved on medication. Intake of food was not related to the pain. He also complained of orthopnea and paraxosmal nocturnal dyspnea.
-no h/o burning micturition
-no h/o reduced urine output
-no h/o itching or rash.
-h/o reccurent high grade fever for 4 days 6 days back with chills and rigors only during the presence of fever and was not relieved on medication.
-no h/o cough with sputum.
-no h/o constipation.
-no h/o diarrhea.
-no h/o headache, blurring of vision.
- no loss of consciousness.
Earlier daily routine —
Earlier when the patient was asymptomatic he used to begin the day at 6am and used to work in the shed.
At 9am he used to eat breakfast which consisted of rice and tea.
Then he used to go to the farm and eat lunch at around 1pm which again consisted of rice which he used to consume at the farm only.
Around 9pm he used to have dinner containing rice and goes off to sleep.
Current daily routine —
In the morning at around 7am he eats 2 idles. At around 11am he eats a little rice and at around 8pm eats a little quantity of rice again and goes off to sleep.
ASSOCIATED DISEASES:
———
PAST HISTORY:
No K/C/O HTN, DM, TB, Epilepsy, CAD, CKD.
h/o blood transfusions after getting admitted here.
He has had cataract surgery in right eye 3 years back and left eye 1 year back.
PERSONAL HISTORY:
Married.
Resides in Miryalguda.
Farmer by occupation.
On a mixed diet.
Adequate sleep.
Has a reduced appetite.
Normal Bowel movements.
Has no known allergies.
Consumes 1-2 glasses of alcohol everyday since 10 years and 4-5 Sutta everyday for the past 10 years.
FAMILY HISTORY:
- h/o father having HTN and left hemiplegia.
Has N/K/C/O No Strokes. No CAD, TB, Asthma or Epilepsy.
DRUG HISTORY:
GENERAL EXAMINATION:
-Palor present
-No icterus
-No cyanosis
-No lymphadenopathy
-No pedal edema
-No clubbing of fingers
VITALS:
Temperature: Afebrile - 98.9°F
Pulse: 66 beats per minute
Respiratory rate: —18 cycles per minute
Blood pressure: 120/80 mm of Hg
SPO²: 100%
GRBS: 163mg%
SYSTEMIC EXAMINATION:
Cardiovascular system:
No thrills
No murumurs
Cardiac sounds: S1, S2 present
Respiratory system:
No dyspnea
No wheezing
Breath sounds heard: vesicular? yes
Abdomen:
-Shape : Obese
-No Tenderness present
-No palpable mass
-Non palpable spleen
-Non palpable liver
-No free fluid (ascites) present
-No bruits
-Bowel sounds: heard
Central Nervous System:
Conscious and Alert
Speech: Normal
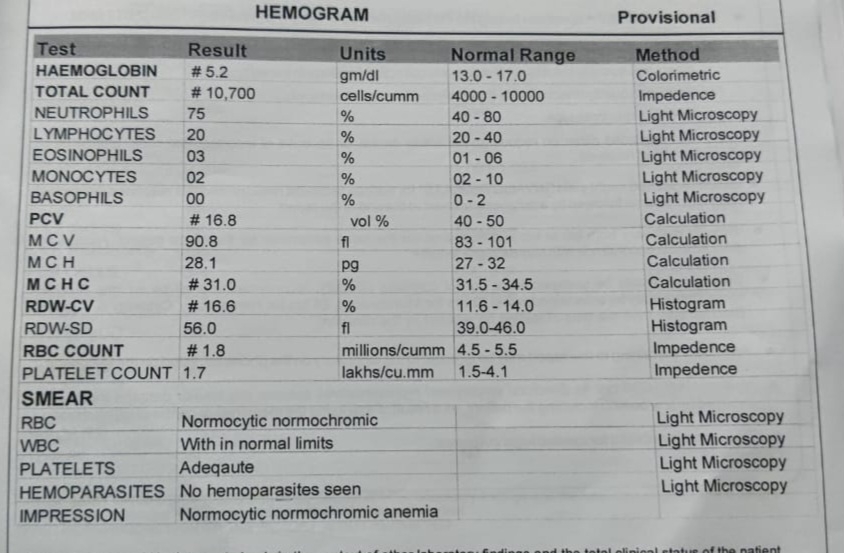
INVESTIGATIONS:
Biochemical investigations:
ECG:
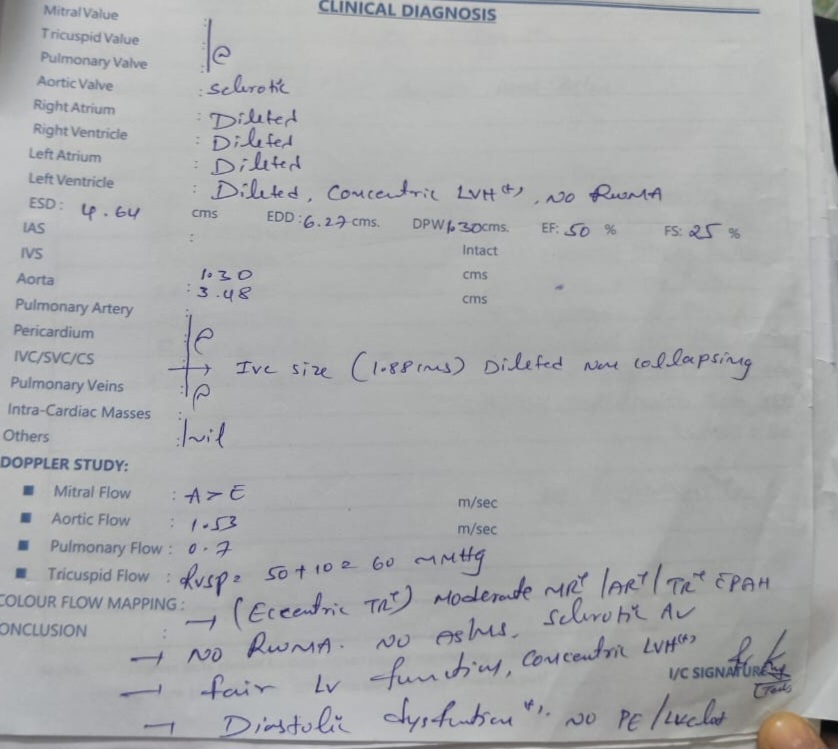
2D-ECHO REPORT:
ULTRASOUND REPORT:
GRAPHIC SHEET :
PROVISIONAL DIAGNOSIS:
———